PPCM Basics
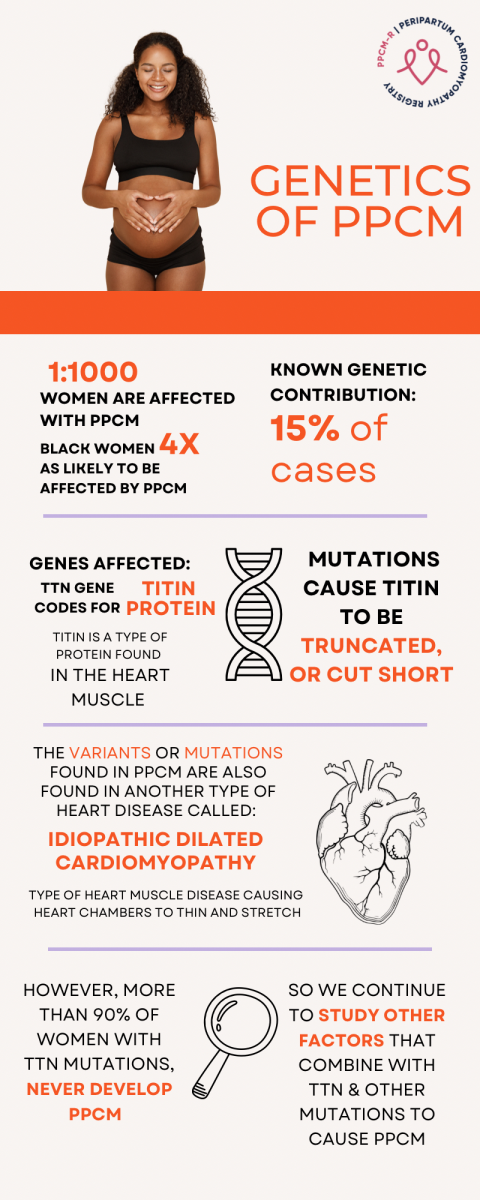
PPCM Fast Facts - Genetics
What is PPCM?
Peripartum cardiomyopathy is a type of heart muscle weakness that occurs near the end of pregnancy or in the months after. The word cardiomyopathy typically refers to a decrease in the function or change in structure of the heart muscle. The heart's pumping function is referred to as the “ejection fraction” which is a term for the percent of blood volume ejected from the heart with each beat. In PPCM, the ejection fraction goes down, which can cause symptoms of heart failure. These symptoms include a build-up of fluid in the lungs leading to shortness of breath and swelling in the legs. In more severe cases, other organs are damaged due to poor blood flow as a result of heart muscle weakness.
What are the symptoms of PPCM?
For many patients, the symptoms of PPCM can be confused with symptoms of pregnancy. The most common symptoms include shortness of breath with activity, fatigue, shortness of breath while lying flat, swelling in the body, particularly legs, chest tightness, and waking up at night due to shortness of breath.
How is PPCM diagnosed?
- A chest X-ray may be done to look for fluid overload within the lungs
- Blood testing, specifically a lab called nt-BNP (or BNP) can detect fluid overload
- An ECG (heart electrical tracing) is often done to look for any cardiac electrical abnormalities
- Echocardiography, an ultrasound of the heart, can detect heart muscle weakness.
When is PPCM diagnosed?
The majority of women with PPCM are diagnosed near the end of pregnancy or in the months after. Sometimes, PPCM is missed as the symptoms are confused with symptoms of pregnancy.
What are common risk factors for developing PPCM?
In the US, black women are much more likely to develop PPCM than white women. Additional risk factors include pre-eclampsia (a type of high blood pressure during of pregnancy, genetic defects, history of cancer, and a pregnancy with multiple babies. The exact cause of PPCM, however, is not entirely understood and continues to be studied.
What are the mainstays of PPCM treatment?
The treatment of PPCM includes many of the medications used in other types of heart failure. Fortunately, several of these medications are safe for pregnancy and breastfeeding. The most common medications used for treatment are described below:
- Loop diuretics commonly referred to as “water pills” allow excess fluid to be excreted as urine. These medications help with the symptoms of fluid overload in PPCM
- Beta-blockers are heart medications that both slow the heart rate and help the heart function improve
- Other heart muscle strengthening medications will be selected based on symptoms and if the patient is pregnant or breastfeeding. Certain medications are not safe during pregnancy or breastfeeding thus it is important for doctors to select medications carefully.
- Anticoagulation, or blood-thinner therapy, is used for patients with severe PPCM. Severe PPCM with pregnancy puts patients at high risk for blood clotting. However, the decision to start these therapies may depend on each individual patient and their risk factors for developing blood clots.
Other therapies may be required in more complicated or severe cases of PPCM. The goal of therapy is to help with symptoms of PPCM and help in the recovery of heart function.
How long does PPCM last?
Fortunately, PPCM patients recover at a higher rate than patients with other forms of heart failure. Nearly half of PPCM recovery occurs within the first 6 months. However, some patients will continue to recover for 1 to 2 years post-diagnosis.
