This is a report of 1 year outcomes from the European Society of Cardiology EURObservational Resaearch PPCM Registry. This registry enrolled women from 51 countries. One year data were availble in 535 women. At 1 year, death occured in 8.4% of enrolled women, this differed significantly by geographic location. 14.0% of women had at least one rehospitalization. At 1 year, 66.1% of women had recovery of LV function.
PPCM Articles
Outcomes at 1 year in women with peripartum cardiomyopathy: Findings from the ESC EORP PPCM Registry
Year Published:
2023
Summary:
Journal:
European Journal of Heart Failure
Abstract:
Year Published:
2023
Summary:
A retrospective reivew of 45 women who had 78 subsequent pregnancies after being diagnosed with PPCM. Adverse outcomes - mainly heart failure and recurrence of PPCM- were more common in women who had a subsequent pregnancy without recovered LV function compared to women who had a subsequent pregnancy with a recovered ejection fraction (53% of subsequent pregnancies in women without recovered ejection fraction compared to 20% of subsequent preganancies in women who had recovered LVEF).
Journal:
Journal of the American College of Cardiology
Abstract:
Year Published:
2016
Summary:
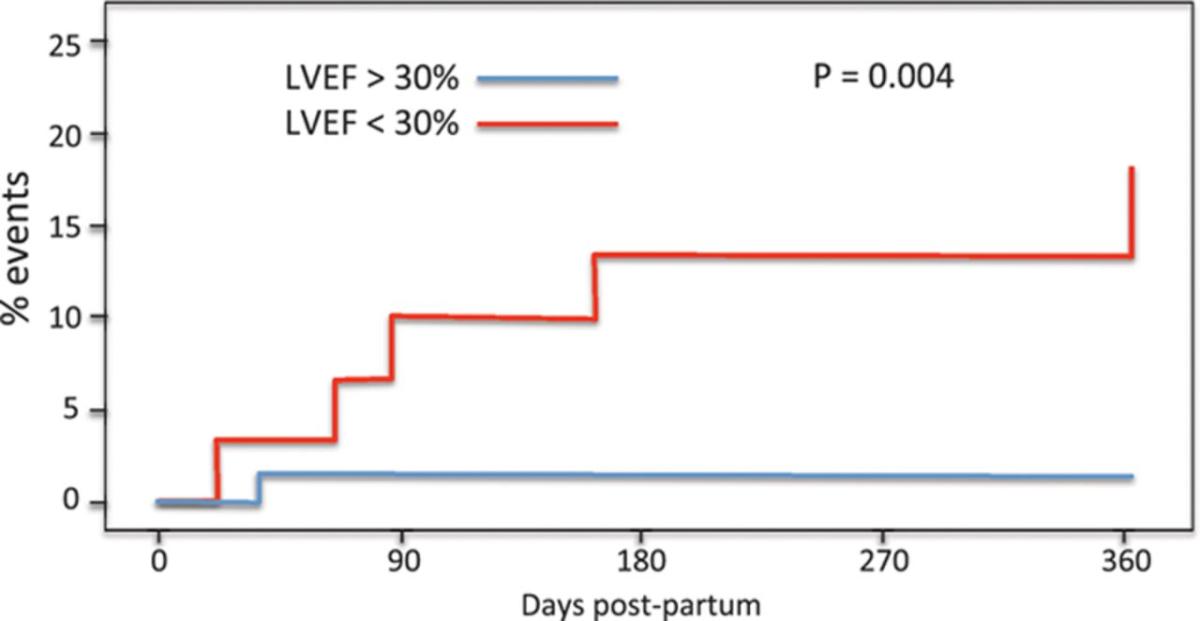
Great review of epidemiology, clinical presentation, and management of peripartum cardiomyopathy. Figure 3 from the article shows data from the IPAC trial which shows that most of the events (heart transplant, death and LVAD) happened in women with intial LVEF of < 30%.
Journal:
Circulation
Abstract:
Year Published:
2020
Summary:
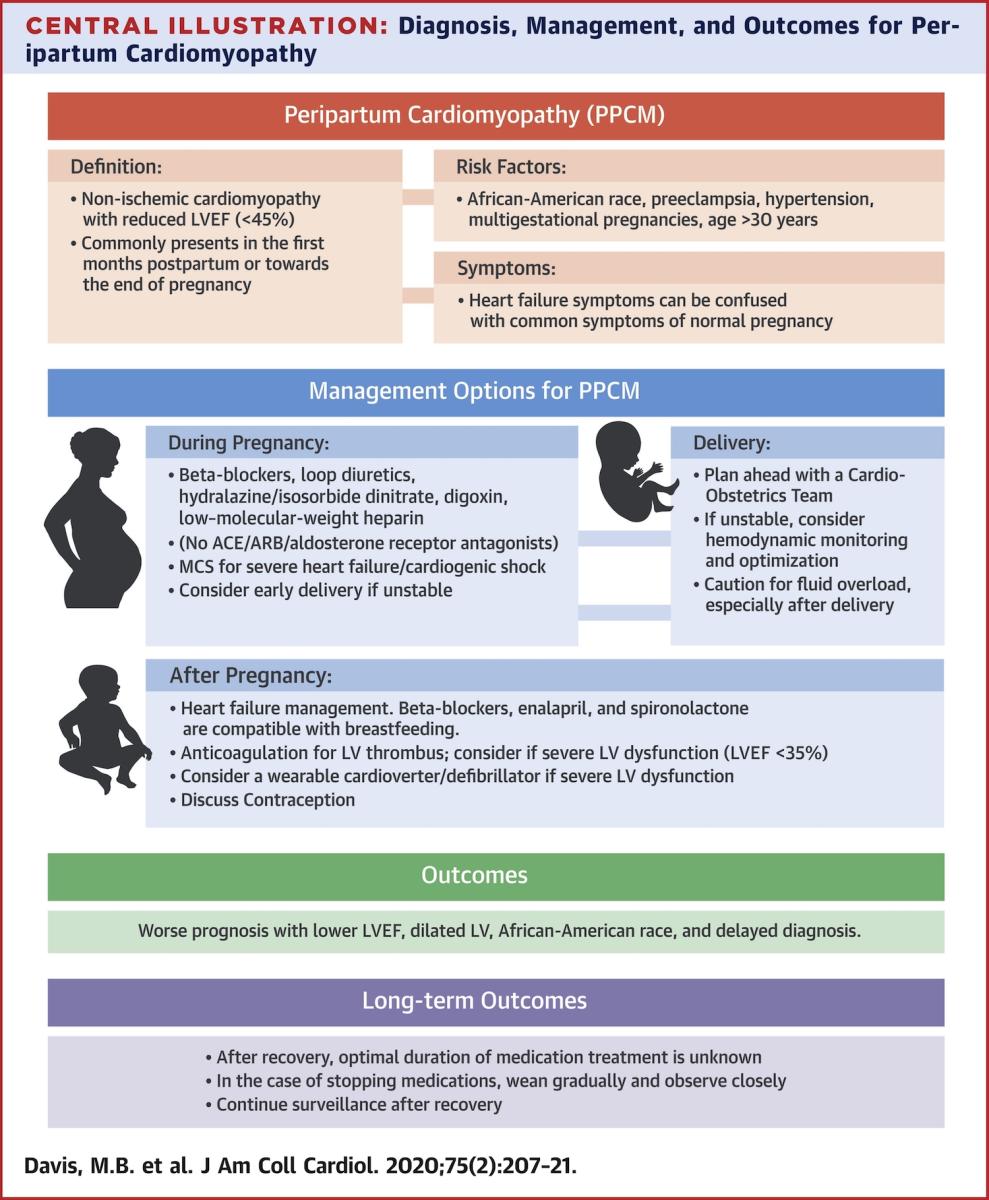
Excellent review article with information on the definition, diagnosis, prognosis and current management of PPCM. The article reviews management recommendations for a subsequent pregnancy after PPCM and discusses cardiovascular medication management during pregnancy and breastfeeding. There are excellent educational figures.
Journal:
Journal of American College of Cardiology
Abstract:
